Evaluating pandemic policies has become a crucial aspect of understanding the multifaceted impacts of COVID-19 interventions. As we reflect on the decisions made during the crisis, such as school closures and lockdowns, it is imperative to assess how these public health policies affected mortality rates and societal wellbeing. Recent analyses reveal that many of these measures, often crucially debated during the pandemic, may not have significantly reduced fatalities while inflicting considerable economic and social harm. Experts argue that a comprehensive pandemic response analysis is necessary to grapple with the long-term implications of our approach to crisis management. By examining the economics of COVID-19 alongside the effects of these interventions, we can pave the way for a more informed discussion about public health strategies in future emergencies.
Assessing the strategies employed during health crises like COVID-19 is vital for learning how to handle future outbreaks effectively. By scrutinizing measures such as enforced isolations and educational institution closures, we can better understand their ramifications on different segments of society. Research indicates that these critical decisions, although made in haste, had profound and enduring consequences that call out for careful examination. It is essential to investigate the broader implications of public health strategies, particularly how they intersect with socioeconomic elements to inform subsequent responses to health emergencies. Analyzing the effectiveness and consequences of these strategies will help to improve protocols and possibly prevent similar mistakes in the future.
Evaluating Pandemic Policies: Lessons from COVID-19
The COVID-19 pandemic has prompted extensive analyses of public health policies implemented globally, particularly non-pharmaceutical interventions like school closures and lockdown measures. Evaluating pandemic policies is crucial for understanding which strategies were effective in mitigating the virus spread while weighing the broader societal impacts. A book by Princeton University professors Frances Lee and Stephen Macedo argues that many of these policies lacked empirical support in improving mortality rates. They highlight that the desire for collective action may have stifled dissenting opinions, ultimately hindering a comprehensive evaluation of pandemic strategies.
As policymakers and public health officials navigate future crises, examining the lessons learned from COVID-19 interventions becomes imperative. The push for sustained accountability demands that we scrutinize the effectiveness of various health measures, not just in theory but in real-world applications. This reflection should include how decisions impacted vulnerable populations, as highlighted in the ACLU’s warnings before the pandemic. As we assess pandemic policies, it’s essential to foster an environment where diverse viewpoints are encouraged, enabling a more thorough understanding of effective public health measures.
The Impact of School Closures on Society
School closures during the COVID-19 pandemic have sparked considerable debate regarding their long-term repercussions on children and their families. With physical classrooms shut down, many children faced educational setbacks that disproportionately affected those from low-income backgrounds. Educational experts have noted significant delays in learning outcomes and a rise in mental health issues among students, suggesting that the consequences of such decisions are far-reaching. As Frances Lee indicated, nearly half of U.S. public schools remained closed well into 2021, a policy that failed to show significant benefits in reducing COVID mortality.
Furthermore, the socioeconomic effects of school closures resonate beyond the classroom. Parents struggled to balance home schooling with work responsibilities, often resulting in increased stress and financial pressure. The long-term effects of these closures could exacerbate existing inequalities as educational disparities widen, particularly for underprivileged groups. Understanding the multi-faceted implications of school closures is vital as we evaluate pandemic responses and prioritize effective, equitable education policies for future public health challenges.
The Economics of COVID-19: Costs and Consequences
The economic ramifications of COVID-19 interventions have raised critical questions regarding resource allocation and fiscal policy. With over $5 trillion authorized in relief spending, the financial burden has dramatically increased public debt, elevating concerns about sustainable economic growth. As outlined by Frances Lee, the rapid increase in federal debt poses significant challenges for future crisis management and long-term economic recovery. Balancing immediate public health needs against the ramifications for national debt will require strategic thinking and accountability.
Moreover, the pandemic has reshaped various sectors, from education to small businesses. Many firms that were forced to shut down faced permanent closures, leading to job losses and economic instability. Communities are grappling with the aftereffects, including empty business districts and increased reliance on government support. Evaluating the economics of COVID-19 necessitates an honest assessment of both the costs and the unintended consequences of lockdowns and school closures. This analysis is critical for developing economic policies that can withstand future public health emergencies.
Public Health Policies: Navigating Future Crises
In light of the COVID-19 experience, public health policies must evolve to better address the complexities of future crises. Transparency, honesty, and open debate among public health officials will be vital in restoring credibility in the field. The authors of “In Covid’s Wake” stress the importance of reassessing the normalized groupthink that characterized decision-making during the pandemic. By fostering healthy discussions around effective strategies, officials can better prepare for unforeseen challenges and implement more robust and inclusive public health measures.
Additionally, it is crucial to prioritize science-based approaches while remaining open to community feedback and concerns. The Great Barrington Declaration illustrated a rift in public health discourse, emphasizing the need for comprehensive review and adaptability in policy-making. Ensuring that future public health strategies are informed by diverse perspectives will not only cultivate public trust but also improve the efficacy of interventions designed to protect population health. Policymakers must learn from the past to better navigate future public health emergencies.
Lessons Learned: The Role of Accountability in Public Health
The COVID-19 pandemic has illuminated the need for accountability in both policy formulation and public health communication. As we reflect on the past, the role of educated elites must be scrutinized—were they accountable for the choices made during the pandemic? The findings presented by Lee and Macedo highlight a failure to engage in critical discourse, which arguably contributed to detrimental decisions regarding lockdowns and restrictions. As the landscape evolves, ensuring accountability can serve as a cornerstone for public health strategy.
Accountability extends to addressing misinformation as well. Public health officials must champion evidence-based practices while confronting ill-informed narratives that undermine community trust. The potential for misinformation amidst public health messaging calls for a reevaluation of communication strategies, making transparency and factual integrity a priority. By fostering a culture of accountability, leaders can establish a framework that promotes resilience and informed decision-making in health crises.
The Value of Open Debate in Public Health Decision-Making
Open debate plays a critical role in enhancing public health decision-making, particularly in the wake of crises like the COVID-19 pandemic. The authors of “In Covid’s Wake” argue for the necessity of discussing dissenting opinions and alternative strategies outside the prevailing rhetoric. Such dialogue is imperative to ensure that policies are not only effective but also considerate of diverse perspectives. By embracing a more inclusive approach to discourse, we can identify innovative solutions that might have been overlooked during the pandemic.
Encouraging active participation from a wide range of stakeholders—including healthcare professionals, policymakers, and the public—can enrich the decision-making process. It also fosters an environment where individuals feel empowered to voice their concerns and alternatives. By acknowledging and addressing varying viewpoints, public health officials can develop a more comprehensive and adaptable response to future public health challenges. Ultimately, open debate serves as a foundation for creating effective policies that are both scientifically sound and socially just.
The Psychological Effects of Lockdown Measures on Communities
The psychological toll of lockdowns and social distancing measures has resonated deeply within communities. The restrictions on social interactions and the abrupt shifts in daily routines have led to significant increases in anxiety, depression, and other mental health challenges. As highlighted in various research studies, young people, in particular, have experienced heightened distress, resulting in a substantial impact on their overall well-being and academic performance. Moving forward, society must prioritize mental health initiatives as an integral part of public health responses.
Understanding the psychological effects of lockdowns also underscores the importance of integrating mental health support into public health policies. Rehabilitation strategies, peer support systems, and access to mental health resources can help mitigate the adverse effects observed during the pandemic. As communities seek to recover, acknowledging and addressing the mental health crises stemming from pandemic response will be crucial in fostering resilience and promoting holistic approaches to health.
Future Preparedness: Building Resilient Public Health Systems
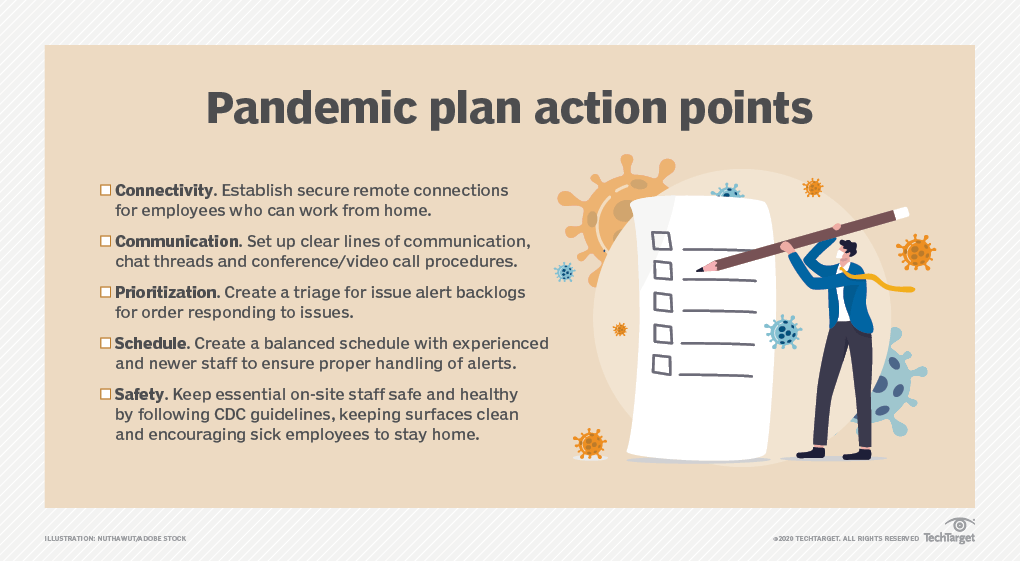
Preparing for future pandemics requires building resilient public health systems capable of swiftly and effectively responding to crises. Lessons learned from the COVID-19 pandemic should inform revisions to existing structures, enabling a more proactive rather than reactive approach to health emergencies. Investments in infrastructure, technology, and training can enhance early detection and response capabilities while minimizing the social and economic impacts observed in 2020.
Additionally, fostering collaboration between governmental entities, healthcare organizations, and communities can enhance resilience. By leveraging shared knowledge and resources, public health systems can develop more effective strategies tailored to unique community needs. As we look to a future marked by potential health challenges, cultivating a robust and adaptable public health framework is essential for safeguarding population health.
Reassessing Community Engagement in Public Health Initiatives
The importance of community engagement has become increasingly evident in public health discourse, particularly during the COVID-19 pandemic. Effective public health measures thrive on the involvement and trust of the communities they aim to serve. As highlighted by the discussions surrounding pandemic responses, a lack of transparency and participation can lead to skepticism and resistance against health policies. Leveraging community input can improve compliance and foster a sense of ownership over health initiatives.
Public health officials must prioritize building relationships with community members to ensure they feel valued and informed. This engagement can take many forms, from public forums to partnerships with local organizations. By actively involving community voices in policy discussions, public health efforts can become more effective and responsive to the needs of the population. Ultimately, reassessing community engagement strategies is crucial for enhancing public trust and achieving better health outcomes.
Frequently Asked Questions
How should we evaluate COVID-19 interventions like school closures and social distancing?
Evaluating COVID-19 interventions, such as school closures and social distancing measures, requires a careful analysis of their effectiveness in reducing mortality rates and the lasting societal impacts they had. Experts argue that many of these non-pharmaceutical interventions may not have achieved their intended outcomes, while causing significant harm to vulnerable populations, particularly children from low-income families.
What are the economic implications of public health policies implemented during the pandemic?
The economic implications of public health policies enacted during the pandemic, such as strict lockdowns and extensive funding, have been profound. The U.S. saw over $5 trillion in COVID relief spending, leading to a substantial increase in public debt from 80% to over 100% of GDP. This financial strain constrains future economic responses, impacting various societal sectors.
What lessons can we learn from the pandemic response analysis regarding dissent in public health policy?
The pandemic response analysis stresses the importance of dissent and open debate in shaping effective public health policies. Many experts argue that the suppression of divergent views during the COVID-19 crisis led to a collective unwillingness to scrutinize the efficacy of policies like lockdowns and mask mandates, ultimately hindering a comprehensive evaluation of their impacts.
How do school closures affect educational outcomes in future pandemic planning?
School closures during the COVID-19 pandemic significantly hindered educational outcomes, with many children facing setbacks that could influence their future academic achievements. Future pandemic planning should consider the long-term effects of such closures, particularly on younger students and those from disadvantaged backgrounds, to improve resilience in future crises.
What strategies can be employed to improve public health policies after evaluating pandemic outcomes?
Improving public health policies after evaluating pandemic outcomes involves fostering transparency, encouraging open dialogue among experts, and incorporating evidence-based practices. Policymakers should allow for candid discussions about the costs and benefits of interventions like lockdowns, to enhance public trust and prepare more effectively for future public health emergencies.
What role does groupthink play in evaluating pandemic policies?
Groupthink can impede the evaluation of pandemic policies by discouraging dissent and critical analysis among experts. This phenomenon was evident during the COVID-19 crisis, where prevailing narratives often silenced alternative viewpoints, ultimately affecting the robustness of policy debates and assessments.
Are there specific metrics to consider when analyzing the impact of pandemic response measures?
Yes, specific metrics to consider when analyzing pandemic response measures include mortality rates, economic stability, educational attainment losses, mental health outcomes, and public trust in health authorities. These metrics help gauge the overall effectiveness and repercussions of interventions like school closures and social distancing.
How can we ensure honesty in public health communications post-pandemic?
Ensuring honesty in public health communications post-pandemic involves fostering a culture of transparency among health officials, where the limits of knowledge and uncertainties surrounding health measures are openly discussed. This can help build public trust and facilitate more informed decision-making during future health crises.
What is the significance of the Lancet study regarding COVID-19 interventions?
The significance of the Lancet study regarding COVID-19 interventions lies in its findings that challenge the effectiveness of measures like school closures and stay-at-home orders in significantly reducing mortality rates. This reinforces the need for thorough assessments and willingness to critique public health strategies employed during the pandemic.
How can we better prepare for future pandemics based on past public health policy evaluations?
To better prepare for future pandemics, it’s crucial to conduct comprehensive evaluations of past public health policies, adopting a flexible approach that allows for rapid assessment and adjustment of strategies as new evidence emerges. Incorporating diverse expert opinions and prioritizing the welfare of vulnerable populations will be vital in shaping effective responses.
| Key Points | Details |
|---|---|
| Pandemic Policy Failures | Non-pharmaceutical interventions like school closures did not effectively reduce mortality rates, causing lasting societal harm. |
| Groupthink and Dissent | Public debates were suppressed, with dissent perceived as morally premature during the pandemic. |
| Loss of Educational Opportunities | Prolonged school closures led to significant educational setbacks, particularly affecting low-income children. |
| Financial Consequences | Over $5 trillion in COVID relief spending has led to persistently high public debt. |
| Need for Open Debate | Future policies must prioritize transparency and diverse viewpoints to avoid similar failures. |
| Impact of Governance | Analysis showed no significant difference in outcomes between blue and red states regarding school and shutdown policies. |
Summary
Evaluating pandemic policies remains crucial for understanding the true impact of government actions during the COVID crisis. The recent revelations about the ineffectiveness of lockdowns and school closures highlight the urgent need for a reevaluation of how these policies were implemented and the consequences they incurred. Moving forward, it’s imperative that we embrace open dialogue and acknowledge diverse opinions to ensure more balanced decision-making in response to future public health crises.